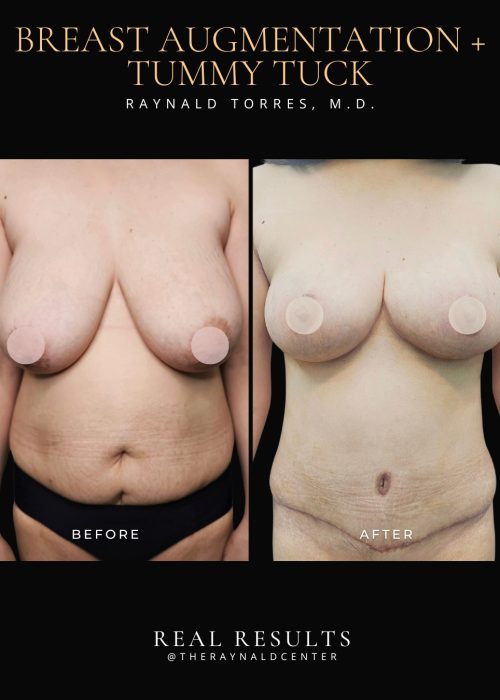
Tummy Tuck
BEFORE AND AFTER
What is Tummy Tuck?
A tummy tuck, or abdominoplasty, is designed to restore a flatter, firmer, and more contoured abdomen — especially after pregnancy or significant weight loss. It addresses not only excess skin and fat, but also the separation of abdominal muscles (diastasis recti), which is common after pregnancy.
This procedure is a key component of a mommy makeover. Many women find that despite diet and exercise, the tummy area doesn’t return to its pre-pregnancy state. The abdominal wall becomes weak, and skin loses its elasticity.
A tummy tuck allows me to tighten the core by repairing the underlying muscles and removing loose skin and fat for a more toned midsection. The incision is placed low along the bikini line and is carefully designed to be hidden under underwear or swimwear. I often combine it with liposuction to shape the waist and flanks for an even more refined silhouette.
The decision between a tummy tuck and just liposuction depends on the quality of your skin. If your skin is still elastic and firm, liposuction alone may be enough — the skin will naturally shrink to your new shape. But if there’s significant skin laxity or sagging, a tummy tuck may be the better option to achieve smoother, tighter results. For select cases, I also offer an apron lift, which is a procedure that removes excess lower abdominal skin after liposuction without repositioning the belly button. This can be a great choice if there’s mild to moderate skin redundancy and you want a faster recovery time.
Patients often ask when the right time is to have this done — I usually recommend waiting at least one year after giving birth, when your body has healed, you’re no longer breastfeeding, and your weight has stabilized. For long-term satisfaction, it’s also best if no future pregnancies are planned, as this could stretch the abdominal wall again.
The result is not just cosmetic — many patients tell me they feel stronger, more confident, and more comfortable in their clothes. A tummy tuck helps restore not just your shape, but your confidence.
Pre-Procedure Guidelines
Proper preparation helps minimize risks and supports smooth recovery.
1. Medical Preparation
Complete all required laboratory tests and medical clearance.
Inform your surgeon of any medical conditions (e.g., diabetes, hypertension), allergies, or medications you are currently taking.
Stop blood-thinning medications (aspirin, ibuprofen, herbal supplements) 7 days before surgery, unless directed otherwise.
Continue your maintenance medications unless your doctor instructs you to stop them.
2. Lifestyle Adjustments
NO smoking or vaping at least 2 weeks before and after surgery, as nicotine reduces blood flow and impairs healing.
NO alcohol for at least 48 hours before the procedure.
Arrange for a companion to drive you home and assist you during the first 48–72 hours post-op.
Prepare loose, comfortable clothing and a post-surgical binder or compression garment as advised.
3. Day of Surgery
Do not eat or drink anything (not even water) 8 hours before surgery if general anesthesia will be used.
Shower using antibacterial soap the night before and morning of surgery.
Remove all makeup, nail polish, jewelry, and contact lenses.
Wear loose, front-opening clothes.
Post Procedure Guidelines
Following your post-op instructions carefully will help reduce complications and ensure a smoother recovery.
1. Activity & Movement
Start gentle walking around your home as soon as possible to promote circulation and reduce the risk of blood clots.
Do not stand fully upright for about 7–10 days; keep your back slightly bent while walking and sleep with your knees slightly bent and head elevated.
Avoid strenuous activity, bending, lifting, or core exercises for 4–6 weeks.
2. Compression Garment
Wear your abdominal binder/compression garment 24 hours a day for the first 2–3 weeks, then during daytime for up to 6–8 weeks.
This helps reduce swelling, support healing tissues, and shape your waistline.
Remove only during brief showers or as advised by your surgeon.
3. Wound Care
Dressings may be removed after 48 hours or as advised. Do not remove steri-strips or surgical tape unless instructed.
Clean the wound area gently using distilled water and cotton buds. Keep incisions dry and clean.
You may take a gentle shower after 2–3 days, but avoid soaking the wound area (no baths or swimming).
4. Medications
Take all prescribed medications, including antibiotics and pain relievers, as directed.
Do not take aspirin or NSAIDs unless approved by your surgeon.
Resume maintenance medications for existing conditions unless advised otherwise.
5. Lifestyle Restrictions
Avoid smoking and alcohol for at least 2–3 weeks post-op to prevent delayed healing and complications.
Avoid constipation by drinking plenty of water and consuming fiber; stool softeners may be prescribed.
Maintain a healthy diet to support healing.
6. Pain, Swelling & Healing
Swelling, bruising, and mild to moderate pain are normal and will subside over a few weeks.
Numbness around the incision area may occur and typically resolves gradually.
Drainage tubes, if placed, will be removed during follow-up. Monitor for any foul-smelling discharge, pus, or excessive redness, and contact your surgeon if observed.
7. Sleep Position
Sleep in a semi-reclined position using multiple pillows or a recliner for at least 7–10 days.
Keep your knees slightly bent to reduce tension on the incision site.
8. Follow-Up Appointments
Attend all scheduled follow-up visits to ensure your incision is healing properly and no complications are developing.
Your surgeon will advise when it’s safe to resume more physical activities.