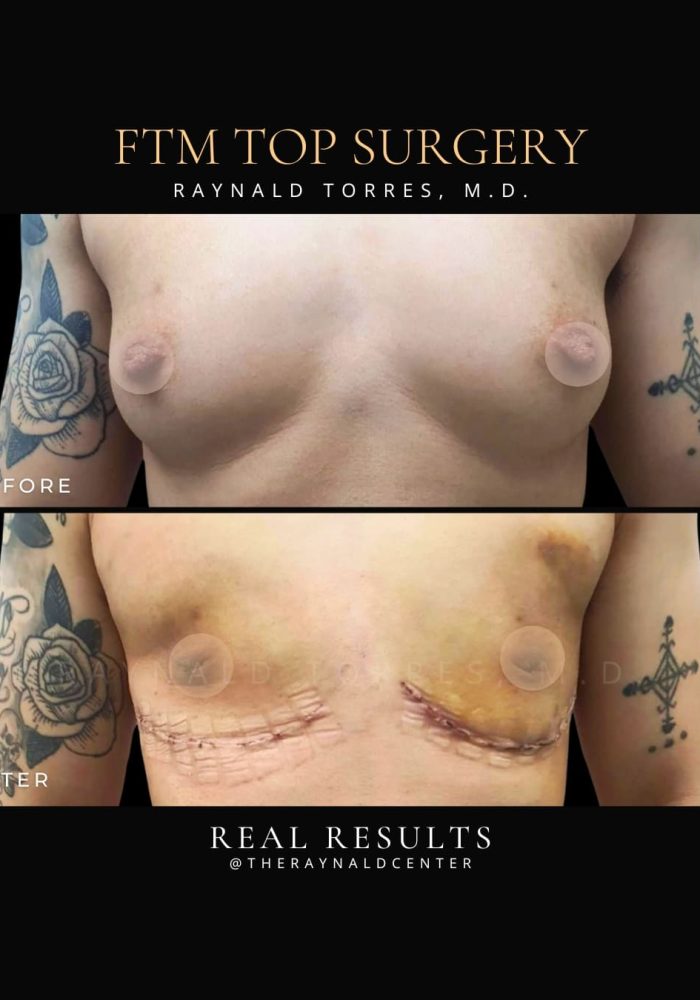
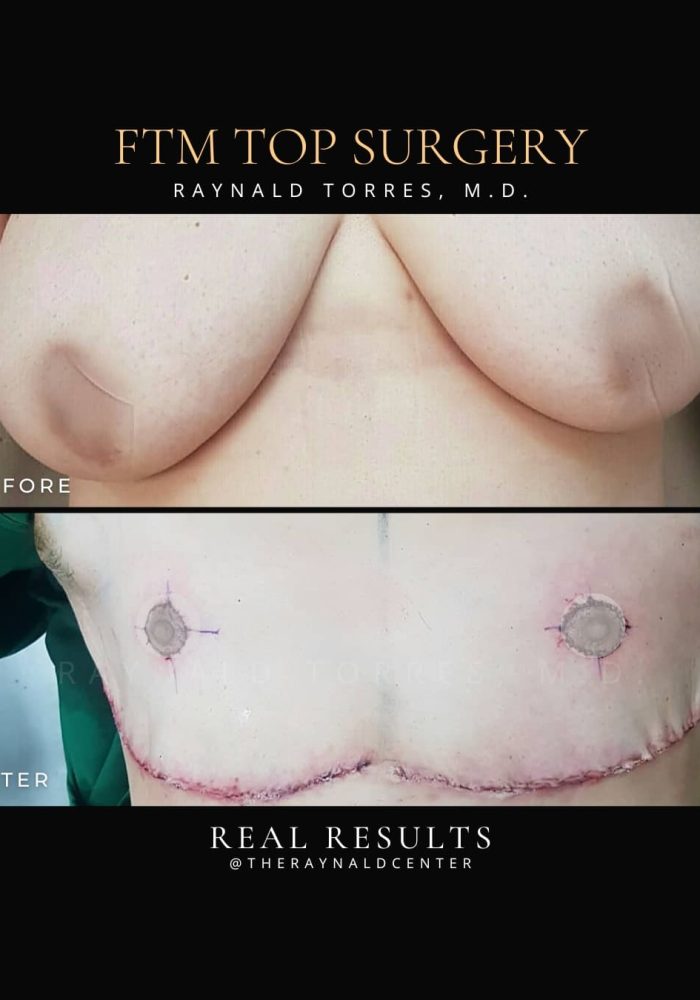
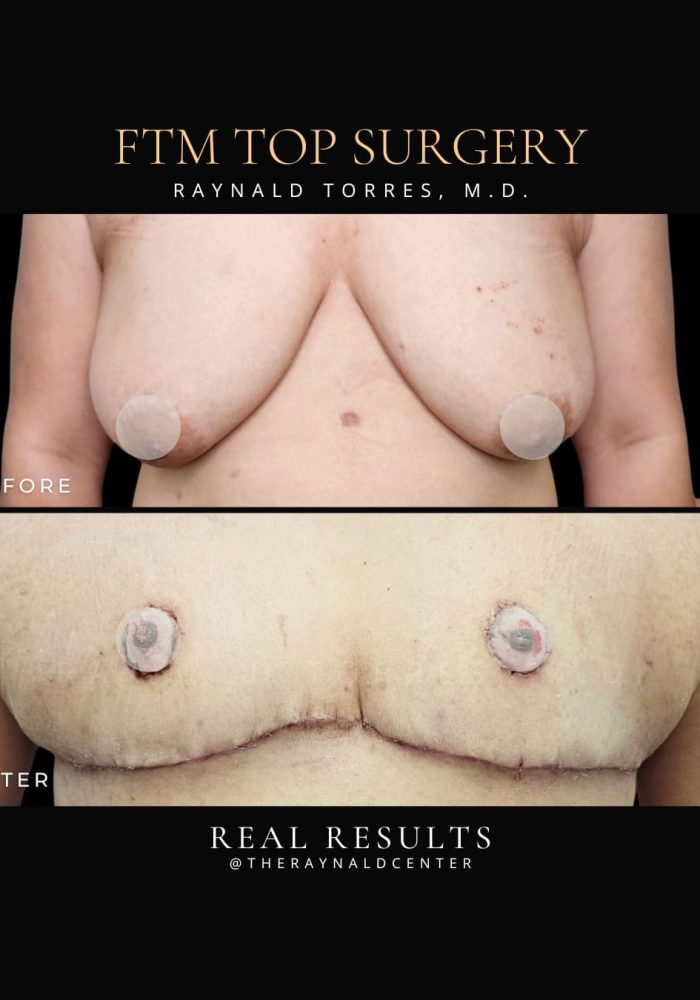
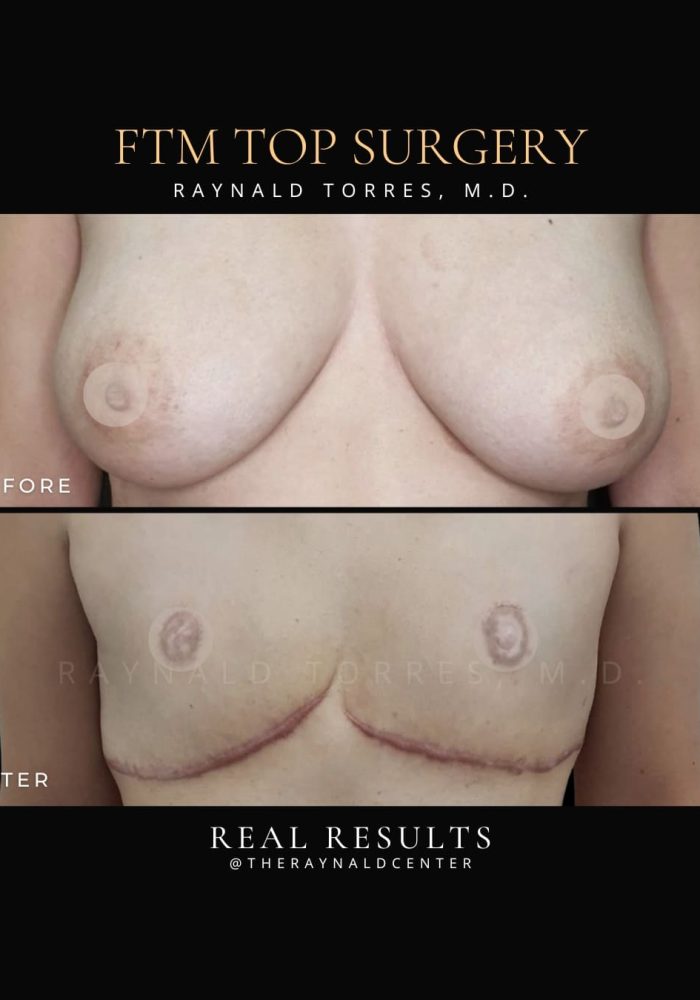
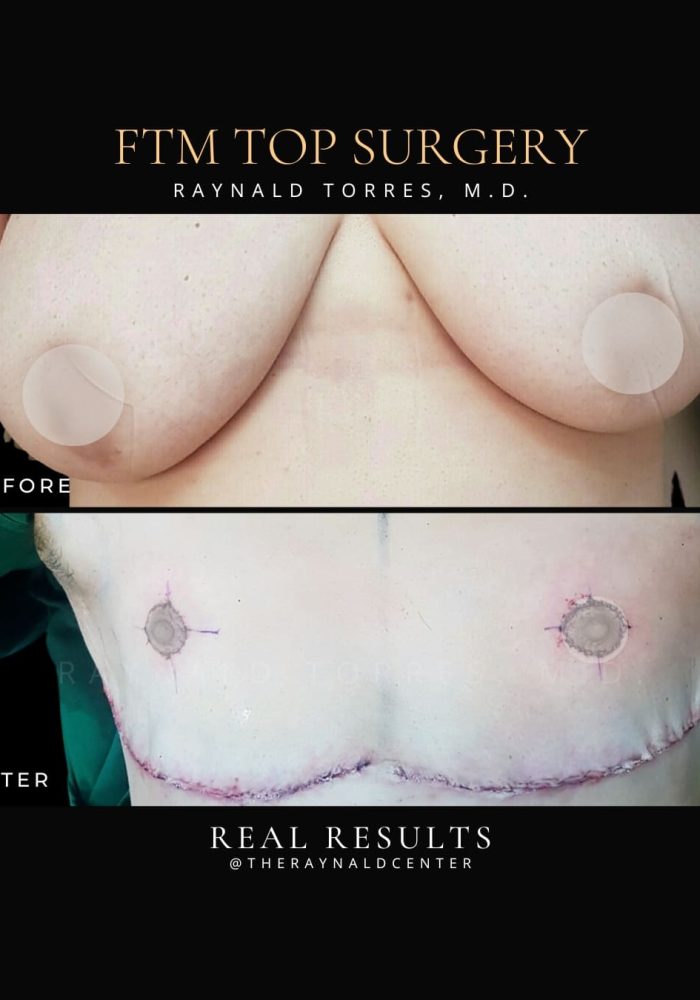
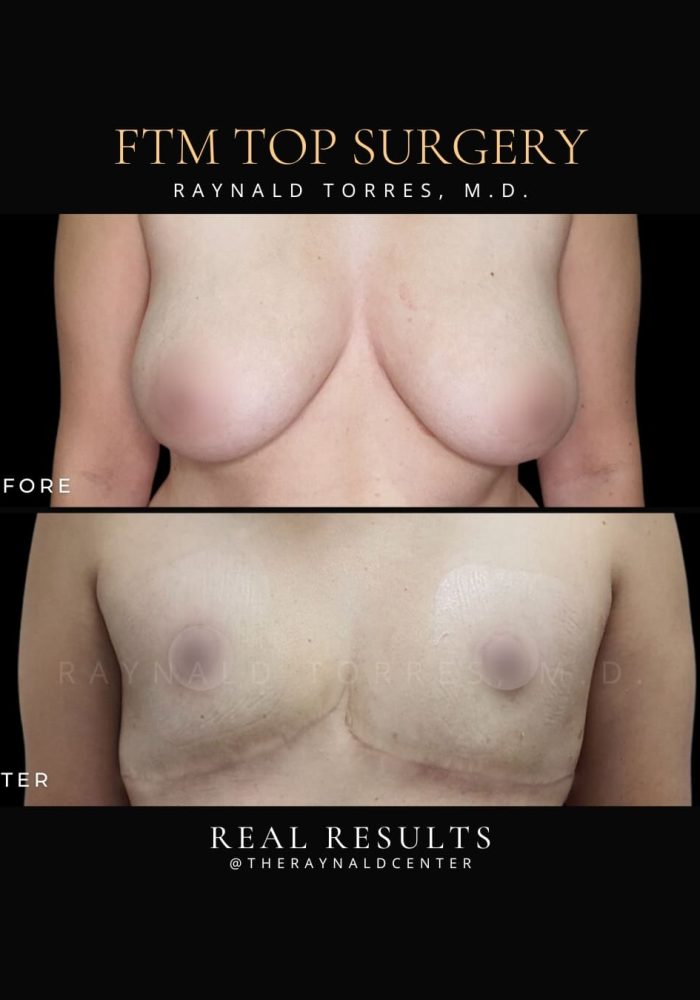
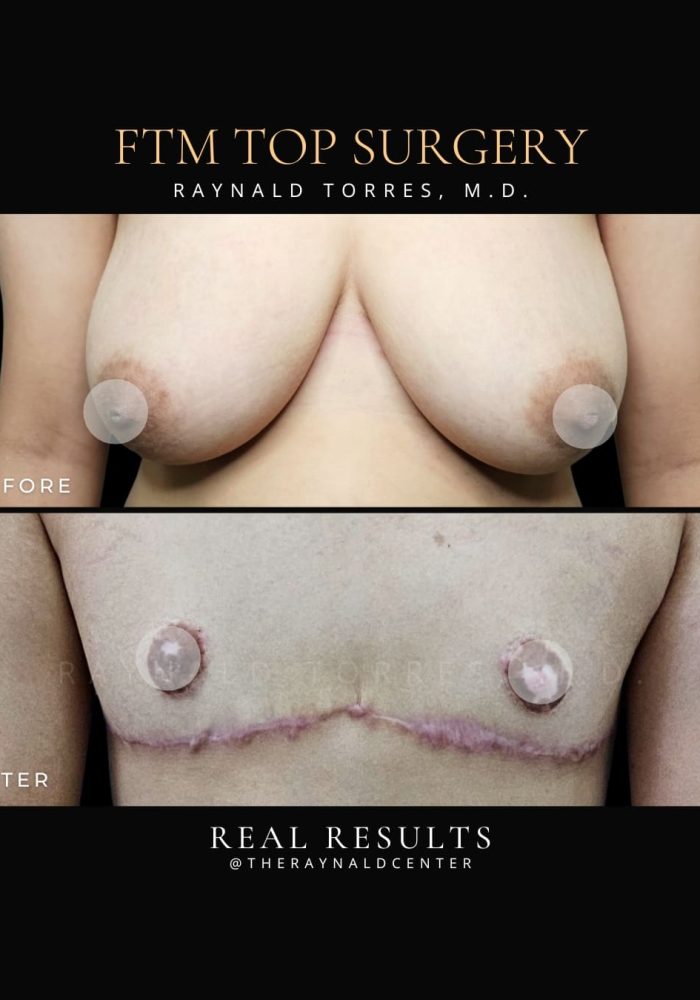
Female-to-Male (FTM) Top Surgery for Gender Reaffirmation
BEFORE AND AFTER
videos
What is Female-to-Male (FTM)?
FTM top surgery is a transformative procedure that helps individuals transition to a more masculinized chest appearance, providing both physical and emotional benefits. My approach to FTM top surgery is centered on achieving natural, aesthetically pleasing results, while ensuring that the patient feels confident and comfortable with their new chest contour.
Double Incision with Free Nipple Grafting
The technique I use for FTM top surgery is the double incision with free nipple grafting, which is ideal for patients with a larger chest or excess breast tissue. This approach involves making two horizontal incisions along the lower chest, which allows me to remove the breast tissue and contour the chest to create a more masculine shape. The free nipple grafting technique is used to reposition the areola and nipple onto the newly contoured chest. This ensures that the nipple is placed in a natural position that is proportionate to the male chest.
The double incision technique allows for more precise control over the chest’s shape and ensures a more defined, masculine appearance. This method also results in well-hidden, inconspicuous scars that are located along the lower chest fold.
Why Double Incision with Free Nipple Grafting?
Suitable for Larger Chests: This technique is highly effective for individuals with larger breasts or more extensive breast tissue. It provides the most optimal results in terms of contouring the chest and ensuring a natural appearance.
Customizable Results: The free nipple grafting method allows for flexibility in positioning the nipple and areola to create a more masculine and aesthetically pleasing look.
Natural-Looking Nipple Placement: Free nipple grafting ensures that the nipple is placed in a location that matches the chest’s new anatomy, making the overall result look more natural and harmonious.
The results of FTM top surgery are permanent, providing a chest that is more in alignment with your gender identity. The scars from the incisions typically heal well, and over time, they become less noticeable, often hidden along the natural chest fold. By using the double incision with free nipple grafting technique, I can achieve results that are both functional and aesthetically natural, ensuring the chest looks masculine and feels like an integral part of the transition.
Pre-Procedure Guidelines
Proper preparation is key to a smooth procedure and optimal recovery.
1. Medical Preparation
Complete all required laboratory tests, imaging, and medical clearance as advised.
A mental health letter supporting your readiness for gender-affirming surgery may be required, depending on local regulations and healthcare standards.
Disclose all current medications, supplements, allergies, and existing medical conditions.
Stop aspirin, NSAIDs, vitamin E, herbal supplements, and other blood thinners at least 7 days before surgery, unless otherwise advised.
2. Lifestyle & Personal Preparation
No smoking or vaping for 2–3 weeks before surgery—this reduces the risk of poor wound healing and scarring.
Avoid alcohol for at least 48 hours before surgery.
Prepare comfortable, front-opening clothing, gauze pads, and your compression binder as instructed.
Arrange for a trusted adult to accompany you and assist for the first 48–72 hours after surgery.
Plan for 2–4 weeks of downtime to allow for healing and limited mobility.
3. Day Before & Day of Surgery
Do not eat or drink anything 8 hours before surgery if general anesthesia is used.
Shower using antibacterial soap the night before and morning of surgery.
Remove all jewelry, nail polish, makeup, and contact lenses.
Wear loose, front-button clothing for easy dressing post-op.
Post Procedure Guidelines
Careful post-op management is essential for healing, comfort, and achieving masculine chest contours.
1. Activity & Movement
Rest for the first 48 hours, but begin gentle walking as soon as tolerated to prevent blood clots.
Avoid lifting arms above shoulder level, lifting heavy objects, or doing household tasks for 2–4 weeks.
Do not resume strenuous physical activity or upper body workouts for at least 6 weeks.
2. Compression Binder
Wear your compression binder 24/7 (except when bathing) for 4–6 weeks, or as directed.
The binder helps minimize swelling, support tissue healing, and maintain chest contour.
3. Drain Care (if applicable)
Drains may be placed to remove excess fluid.
Empty, measure, and record fluid output twice a day.
Follow specific instructions on how to clean and secure drains.
Drains are typically removed within 5–10 days, depending on fluid output.
4. Wound & Scar Care
Leave surgical dressings in place until advised to remove or change them.
After dressing removal (usually within 2–3 days), clean wounds with distilled water and cotton buds.
Keep incisions clean and dry—no baths, pools, or submerging wounds until cleared.
Scar massage or silicone therapy may be recommended after incisions close to improve scar appearance.
5. Bathing
You may shower after 48–72 hours or once drains are removed, depending on your surgeon’s advice.
Pat incisions dry—do not rub.
Avoid getting the binder soaked. Use a clean towel under the binder if needed.
6. Medications & Pain Control
Take all prescribed medications, including antibiotics and pain relievers, as directed.
Continue maintenance medications unless advised otherwise.
Avoid aspirin, NSAIDs, and alcohol for the first few weeks post-op unless cleared.
7. Emotional & Psychological Recovery
Emotional changes are normal during recovery. Feelings of euphoria, sadness, or fatigue can occur due to both physical healing and emotional release.
Reach out to your support system or a mental health provider if needed—this is part of your healing.
8. Follow-Up & Monitoring
Attend all follow-up appointments to monitor healing and manage drains, sutures, or complications.
Contact your surgeon immediately if you experience:
Fever over 38°C (100.4°F)
Signs of infection: pus, foul odor, or excessive redness
Sudden swelling, hardness, or bleeding
Severe pain unrelieved by medication
Shortness of breath or chest pain (seek emergency care)